For thousands of years, a parasite with no name lived happily among horseshoe bats in southern China. The bats had evolved to the point that they did not notice; they went about their nightly flights unbothered. One day, the parasite—an ancestor of the coronavirus, sars-CoV-2—had an opportunity to expand its realm. Perhaps it was a pangolin, the scaly anteater, an endangered species that is a victim of incessant wildlife trafficking and sold, often secretly, in live-animal markets throughout Southeast Asia and China. Or not. The genetic pathway remains unclear. But to survive in a new species, whatever it was, the virus had to mutate dramatically. It might even have taken a segment of a different coronavirus strain that already inhabited its new host, and morphed into a hybrid—a better, stronger version of itself, a pathogenic Everyman capable of thriving in diverse species. More recently, the coronavirus found a new species: ours. Perhaps a weary traveller rubbed his eyes, or scratched his nose, or was anxiously, unconsciously, biting his fingernails. One tiny, invisible blob of virus. One human face. And here we are, battling a global pandemic.
The world’s confirmed cases (those with a positive lab test for covid-19, the disease caused by sars-CoV-2) doubled in seven days, from nearly two hundred and thirteen thousand, on March 19th, to four hundred and sixty-seven thousand, on March 26th. Nearly twenty-one thousand people have died. The United States now has more confirmed cases than any country on earth, with more than eighty thousand on March 26th. These numbers are a fraction of the real, unknown total in this country and around the world, and the numbers will keep going up. Scientists behind a new study, published earlier this month in the journal Science, have found that for every confirmed case there are likely five to ten more people in the community with an undetected infection. This will likely remain the case. “The testing is not near adequate,” one of the study’s authors, Jeffrey Shaman, an environmental-health sciences professor at Columbia University, said. Comments from emergency-room doctors have been circulating on social media like S.O.S. flares. One, from Daniele Macchini, a doctor in Bergamo, north of Milan, described the situation as a “tsunami that has overwhelmed us.”
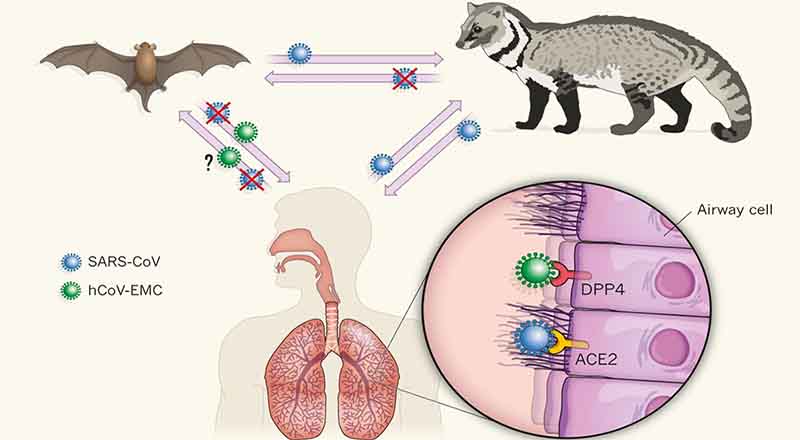
Scientists first discovered that coronaviruses originate among bats following the outbreak of Severe Acute Respiratory Syndrome (sars) in 2003. Jonathan Epstein, an epidemiologist at the EcoHealth Alliance in New York who studies zoonotic viruses—those that can jump from animals to people—was part of a research team that went hunting for the source in China’s Guangdong Province, where simultaneous sars outbreaks had occurred, suggesting multiple spillovers from animals to people. At first, health officials believed palm civets, a mongoose-like species commonly eaten in parts of China, were responsible, as they were widely sold at markets connected to the sars outbreak, and tested positive for the virus. But civets bred elsewhere in Guangdong had no antibodies for the virus, indicating that the market animals were only an intermediary, highly infectious host. Epstein and others suspected that bats, which are ubiquitous in the area’s rural, agricultural hills, and were, at the time, also sold from cages at Guangdong’s wet markets, might be the coronavirus’s natural reservoir.
The researchers travelled through the countryside, setting up field labs inside limestone caverns and taking swabs from dozens of bats through the night. After months of investigation, Epstein’s team discovered four species of horseshoe bats that carried coronaviruses similar to sars, one of which carried a coronavirus that was, genetically, a more than ninety per cent match. “They were found in all of the locations where sars clusters were happening,” he said.
After years of further bat surveillance, researchers eventually found the direct coronavirus antecedent to sars, as well as hundreds of other coronaviruses circulating among some of the fourteen hundred bats species that live on six continents. Coronaviruses, and other virus families, it turns out, have been co-evolving with bats for the entire span of human civilization, and possibly much longer. As the coronavirus family grows, different strains simultaneously co-infect individual bats, turning their little bodies into virus blenders, creating new strains of every sort, some more powerful than others. This process happens without making bats sick—a phenomenon that scientists have linked to bats’ singular ability, among mammals, to fly. The feat takes a severe toll, such that their immune systems have evolved a better way to repair cell damage and to fight off viruses without provoking further inflammation. But when these viruses leap into a new species—whether a pangolin or a civet or a human—the result can be severe, sometimes deadly, sickness.
Siddhartha Mukherjee on how the coronavirus behaves inside a patient.
In 2013, Epstein’s main collaborator in China, Shi Zheng-Li, sequenced a coronavirus found in bats, which, in January, she discovered shares ninety-six per cent of its genome with sars-CoV-2. The two viruses have a common ancestor that dates back thirty to fifty years, but the absence of a perfect match suggests that further mutation took place in other bat colonies, and then in an intermediate host. When forty-one severe cases of pneumonia were first announced in Wuhan, in December, many of them were connected to a wet market with a notorious wildlife section. Animals are stacked in cages—rabbits on top of civets on top of ferret-badgers. “That’s just a gravitational exchange of fecal matter and viruses,” Epstein said. Chinese authorities reported that they tested animals at the market—all of which came back negative—but they have not specified which animals they tested, information that is crucial for Epstein’s detective work. Authorities later found the virus in samples taken from the market’s tables and gutters. But, because not all of the first patients were tied to the market, nor were they connected to one another, Epstein said, “it raised the question of, well, perhaps those forty-one weren’t the first cases.”
Analyses of the sars-CoV-2 genome indicate a single spillover event, meaning the virus jumped only once from an animal to a person, which makes it likely that the virus was circulating among people before December. Unless more information about the animals at the Wuhan market is released, the transmission chain may never be clear. There are, however, numerous possibilities. A bat hunter or a wildlife trafficker might have brought the virus to the market. Pangolins happen to carry a coronavirus, which they might have picked up from bats years ago, and which is, in one crucial part of its genome, virtually identical to sars-CoV-2. But no one has yet found evidence that pangolins were at the Wuhan market, or even that venders there trafficked pangolins. “We’ve created circumstances in our world somehow that allows for these viruses, which would otherwise not be known to cause any problems, to get into human populations,” Mark Denison, the director of pediatric infectious diseases at Vanderbilt University Medical Center’s Institute for Infection, Immunology, and Inflammation, told me. “And this one happened to say, ‘I really like it here.’ ”
According to researchers at Rocky Mountain Laboratories, some viral particles remain viable up to four hours on copper, twenty-four hours on cardboard, and seventy-two hours on plastic and stainless steel, though the number of viable particles begins to decrease within minutes.
The new coronavirus is an elusive killer. Since people have never seen this strain before, there is much about it that remains a mystery. But, in just the past few weeks, genetic sleuthing, atomic-level imaging, computer modelling, and prior research on other types of coronaviruses, including sars and mers (Middle East Respiratory Syndrome), have helped researchers to quickly learn an extraordinary amount—particularly what might treat or eradicate it, through social-distancing measures, antiviral drugs, and, eventually, a vaccine. Since January, nearly eight hundred papers about the virus have been posted on BIORxiv, a preprint server for studies that have not yet been peer-reviewed. More than a thousand coronavirus genome sequences, from different cases around the world, have been shared in public databases. “It’s insane,” Kristian Andersen, a professor in the Department of Immunology and Microbiology at Scripps Research, told me. “Almost the entire scientific field is focussed on this virus now. We’re talking about a warlike situation.”
There are endless viruses in our midst, made either of RNA or DNA. DNA viruses, which exist in much greater abundance around the planet, are capable of causing systemic diseases that are endemic, latent, and persistent—like the herpes viruses (which includes chicken pox), hepatitis B, and the papilloma viruses that cause cancer. “DNA viruses are the ones that live with us and stay with us,” Denison said. “They’re lifelong.” Retroviruses, like H.I.V., have RNA in their genomes but behave like DNA viruses in the host. RNA viruses, on the other hand, have simpler structures and mutate rapidly. “Viruses mutate quickly, and they can retain advantageous traits,” Epstein told me. “A virus that’s more promiscuous, more generalist, that can inhabit and propagate in lots of other hosts ultimately has a better chance of surviving.” They also tend to cause epidemics—such as measles, Ebola, Zika, and a raft of respiratory infections, including influenza and coronaviruses. Paul Turner, a Rachel Carson professor of ecology and evolutionary biology at Yale University, told me, “They’re the ones that surprise us the most and do the most damage.”
Scientists discovered the coronavirus family in the nineteen-fifties, while peering through early electron microscopes at samples taken from chickens suffering from infectious bronchitis. The coronavirus’s RNA, its genetic code, is swathed in three different kinds of proteins, one of which decorates the virus’s surface with mushroom-like spikes, giving the virus the eponymous appearance of a crown. Scientists found other coronaviruses that caused disease in pigs and cows, and then, in the mid-nineteen-sixties, two more that caused a common cold in people. (Later, widespread screening identified two more human coronaviruses, responsible for colds.) These four common-cold viruses might have come, long ago, from animals, but they are now entirely human viruses, responsible for fifteen to thirty per cent of the seasonal colds in a given year. We are their natural reservoir, just as bats are the natural reservoir for hundreds of other coronaviruses. But, since they did not seem to cause severe disease, they were mostly ignored. In 2003, a conference for nidovirales (the taxonomic order under which coronaviruses fall) was nearly cancelled, due to lack of interest. Then sars emerged, leaping from bats to civets to people. The conference sold out.
sars is closely related to the new virus we currently face. Whereas common-cold coronaviruses tend to infect only the upper respiratory tract (mainly the nose and throat), making them highly contagious, sars primarily infects the lower respiratory system (the lungs), and therefore causes a much more lethal disease, with a fatality rate of approximately ten per cent. (mers, which emerged in Saudi Arabia, in 2012, and was transmitted from bats to camels to people, also caused severe disease in the lower respiratory system, with a thirty-seven per cent fatality rate.) sars-CoV-2 behaves like a monstrous mutant hybrid of all the human coronaviruses that came before it. It can infect and replicate throughout our airways. “That’s why it is so bad,” Stanley Perlman, a professor of microbiology and immunology who has been studying coronaviruses for more than three decades, told me. “It has the lower-respiratory severity of sars and mers coronaviruses, and the transmissibility of cold coronaviruses.”: newyorker.com