Nipah Virus infection is a newly emerging zoonotic disease causing severe illness and high fatality in animals and humans. Nipah virus was initially discovered when it caused an outbreak of brain fever among pig farmers in Malaysia in 1998, where pigs were the intermediate hosts. In 2004, cases were reported in Bangladesh, people who consumed date palm sap contaminated by urine or saliva of infected fruit bat. There is no effective antiviral therapy for this infection.
The symptoms of a Nipah Virus infection initially are non-specific and asymptomatic in some people, in others it can present as fever, headache, muscle pain, abdominal pain, nausea, fainting, vomiting and as Respiratory illness. The disease can rapidly progress to coma within 24 to 48 hours in case of encephalitis. Long term sequelae like persistent convulsions and personality changes can also occur.
Nipah Virus is transmitted from bats to humans by consumption of food contaminated by body fluids from infected fruit bats. Pigs are intermediate host. Humans can contract infection from a pig with active disease by coming in close frequent contact, handling raw meat from infected animal or consuming poorly good meat. Human to human transmission has also been known to occur, mostly in family and caregiver of the infected patients.
Precautions to be taken to avoid the spread of Nipah Virus infection –
• Do not consume food contaminated by bat body fluid or bat urine / faeces.
• Do no drink toddy brew in open containers near palm trees.
• Avoid close and frequent contact with an infected person. Following good hygienic practices like washing hands before eating and regularly after visit to public places and hospital is recommended.
• Avoid close physical contact with patients suspected to have Nipah virus infection. Do no share utensils, clothes, restrooms used by an infected person.
• Health care providers who treat infected persons should wear protective gear- gowns and face masks.
Nipah virus infection diagnosed through Real time polymerase chain reaction (RT-PCR) test is done on throat and nasal swabs, cerebrospinal fluid, urine and blood health with diagnosis of infection in early stages.
Diagnosis by detecting antibodies against the virus usually is possible in the 2nd week of illness, the test however is not commonly available. Tissue diagnosis by culture or immunohistochemistry is also possible though available only in select places.
There is no effective treatment available for Nipa virus. Treatment includes symptomatic and supportive care. Strict infection control practices and proper barrier precaution can help to cut back on disease spread.
Prevention is better than cure, hence Avoid contact with pigs and pig handlers. Maintain personal hygiene and intensive hand washing practices. Avoid consuming raw fruits, consume only well cooked, clean, homemade food till the outbreak settles down. Preferably use masks and other barrier precautions while travelling or working in public places that have reported cases of the infection. Be aware of the symptoms and report to the doctor immediately for early diagnosis and treatment.
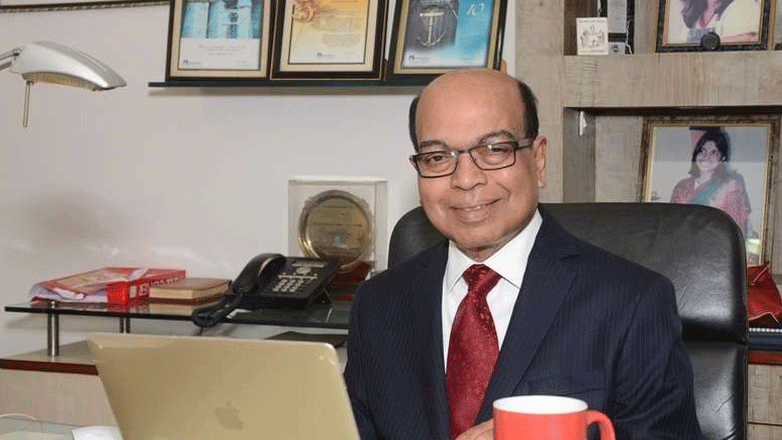
By Dr. VidyaJagadeesan, Consultant – Infectious Diseases, Columbia Asia Hospital, Whitefield